The post You Really Are What You Eat appeared first on Talia Zenlea.
]]>You Really Are What You Eat: Can Food Actually Have an Impact on Health and Disease?
I get a lot of questions from patients about food. There’s a lot of interest lately in using food to treat disease. Now, we know that “eating right” is “healthier” in that too much of anything can make us gain weight, and being obese can put us at risk for heart disease and diabetes, for example. But more and more people are asking me if certain foods can reduce inflammation in the body, reduce cancer risk, and actually change their risks for certain diseases – not just based on the caloric content and impacts on their weight.
Along those same lines, I am seeing more and more patients who tell me that a certain dietary change had a major impact on something totally unrelated and unexpected – like their otherwise hard to treat skin condition, or their child’s behavior in school.
Is there any validity to this?
Though the temptation is to dismiss these associations as coincidence, our growing understanding of the human microbiome has opened our eyes to ways in which food might possibly have a major impact on determining our health and disease states.
What is the microbiome?
The human microbiome is the genetic blueprint of all the organisms (viruses, bacteria, fungi, etc – also called microbiota) that live within the human body. Typically, we think of “bugs” as causing infections. But there are a few areas in our bodies that organisms call home, such as the gut, vagina, lungs, and skin. They feed off of our bodies, and often help us out in various ways in exchange. In recent years, there have been efforts in Europe, the US, and China to sequence and characterize the human microbiome. And what we’ve found is that it’s rich and diverse. You thought humans had a lot of genes? The human microbiome has at least 30 times the number of genes as the human genome!
So now that the human microbiome has been sequenced, the next step is to slowly understand what all the different genes and organisms do.
What determines a person’s microbiome?
The specific organisms living in a person’s gut and the genes that those organisms carry are different from those found in that same person’s lungs, and different from those found in another person. But we’ve noticed that there are also a lot of commonalities. And the people who have more similar microbiota to one another tend to either be related, or live near each other. We’ve also noticed that people who have the same illnesses also have similar changes in their microbiome.
No one knows exactly what determines a person’s microbiome, but we know it’s complicated. It’s likely a combination of genetics and environmental determinants. We know that antibiotics and chronic inflammation can alter the microbiome, as can food.
So why does this matter? Well, it’s hard to change our genetics, and often hard to change a lot of things in our environment. But we can change what we eat, and in turn manipulate our microbiome.
Why does our microbiome impact our health?
As we begin to understand the role of the different microbiota, we’re starting to understand the important role the microbiome plays in maintaining the “status quo” of our bodies. We’re also starting to see that these organisms play a role in how our bodies develop immunity and mediate inflammation.
For example, some of the genes in some of the organisms in our gut are responsible for allowing our bodies to digest certain foods. Without these genes or these organisms, we would not be able to digest these foods. This would be both a nuisance because we would feel sick or bloated when we ate them, but would also lead to significant nutritional deficiencies if these foods were supposed to be major parts of our diets. So why is this concept unique? Because that isn’t our genes that allow us to digest our food – it’s a gene that belongs to a bacteria, that lives inside of us.
On the negative, some of the microbiota in our guts are responsible for releasing from our foods certain compounds that can signal tumours and cancers to grow. Again – these aren’t our genes doing this – these are genes that belong to a bacteria, living in our gut.
I know what you’re wondering – if certain organisms cause inflammation and cancer, and others are good and promote health, why can’t we just eat differently and create a more favourable microbiotic environment?
Food as Medicine?
Believe it or not, this is concept that isn’t far off. We already know that taking antibiotics can decrease the richness of the gut microbiota and can lead to overgrowth of a bacteria called clostridium difficile, that can lead to a severe diarrheal illness. We also know that repopulating the microbiota can treat a stubborn clostridium difficile infection – we do this by transplanting stool from an uninfected person into a person with the infection. A less dramatic example is using a probiotic to treat infectious diarrhea or irritable bowel syndrome.
We know that people with fewer species making up their microbiota have more obesity, diabetes, high cholesterol, and inflammation. We also know that diets with more fiber, fruits, and vegetables lead to a richer microbiome. And we’ve shown a positive association between diets high in fiber, fruits, and vegetables, and a lower risk of inflammatory bowel disease.
What next?
The problem is, we have a lot we still need to understand about the human microbiome, and the complex role it has in health and illness. We need to recognize that the microbiome is only one piece of the puzzle – we also have to contend with different genetic predispositions to certain diseases, and a whole host of other factors. But the more we understand, the closer we are to being able to actually change one major determinant of our health, and we can potentially do that by modifying what we eat.
So for the time being, when people ask me what they can do to “be healthier” – eat a diet high in fiber, fruits, and vegetables. Consider reducing the amount of meat. And most importantly, stay tuned, because in the next few years, we will likely have gained a much better understanding of how to use food as medicine. But for now, there are very few conditions we can treat with diet alone. That being said, when people come in telling me that changing their diet lead to a major improvement in a symptoms or condition they have, I believe it! And I think it’s likely because they changed their microbiome.
The post You Really Are What You Eat appeared first on Talia Zenlea.
]]>The post Highlight on Hiatal Hernia appeared first on Talia Zenlea.
]]>
I get asked about hiatal hernias a lot – what are they, can they be fixed, and most importantly, are they the cause of my symptoms.
Chances are, if you’ve been told you have a hiatal hernia, it’s because you underwent some sore of upper-GI investigation, like an endoscopy or barium swallow, as part of a work-up for symptoms. There’s no way a hiatal hernia can be diagnosed just be looking at you or through a regular physical exam. So it’s no surprise that most people who know they have a hiatal hernia also tend to have upper GI symptoms, like heartburn, pain or trouble swallowing. This can sometimes lead people to conclude that the hiatal hernia must be responsible for the symptoms – because everyone else on the online forum with a hiatal hernia also has symptoms.
It’s important to remember that hiatal hernias are very common, and most often are totally asymptomatic. Here’s what you need to know about hiatal hernias.
What is a hiatal hernia?
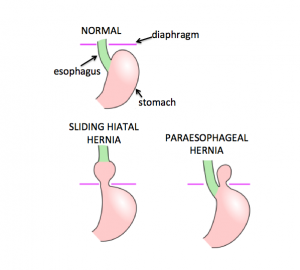
The diaphragm is layer of muscles, that acts as a divider between the chest and the abdomen (like the floor of the chest cavity and the ceiling of the abdominal cavity). The esophagus is the swallowing tube that runs from your mouth to you stomach, meaning it passes through the chest to end up in the abdomen. In order to allow the esophagus through, there’s an opening in the diaphragm, known as the hiatus. Think of it like those pole firefighters slide down (that’s your esophagus), and the hole in the floor of the upstairs to allow the pole to extend to the floor below. Typically, the stomach sits right below the diaphragm (in the “downstairs” abdominal cavity). In people with a hiatal hernia, a part of the stomach pushed up through the hole in the diaphragm. Most of the time, this is because unlike the firefighter’s pole, the esophagus isn’t fixed, and can slide up and down a little bit, bringing the stomach along for the ride. This is called a sliding hiatal hernia. In rare cases, the top of the stomach can push up through the hole in the diaphragm, along side the esophagus. This is a more serious condition called a paraesophageal hernia. Since paraesophageal hernias are pretty uncommon, for the purposes of this discussion, when I refer to a hiatal hernia, I mean a sliding hernia.
What are some symptoms of a hiatal hernia?
The vast majority of the time, a hiatal hernia causes absolutely no symptoms at all. Some people have hypothesized that a hiatal hernia can worsen symptoms of acid-reflux, because when the top of the stomach slides up above the diaphragm, the diaphragm “pinches” that bubble of tissue, making it hard for the stomach acid to move back down to the lower parts of the stomach, and instead causes them to reflux upwards into the esophagus. Symptoms of acid reflux include heartburn, pain in the chest or stomach, acidic taste or pain in the throat, or trouble swallowing. (But these symptoms are general and can be caused by any number of things – so always discuss symptoms like these with your doctor!).
How is a hiatal hernia treated?
Most of the time, hiatal hernias do not cause symptoms and do not require treatment. If it’s thought that you have symptoms of acid reflux, your doctor may suggest a combination of dietary and lifestyle changes, and/or medications – the same things doctors would suggest whether or not you have a hiatal hernia. To learn more, read about heartburn here.
If you have an exceptionally large hiatal hernia that’s causing a lot of trouble, your doctor may recommend that it be corrected. The only way to do this is with an operation to pull the stomach down and prevent it from going back up.
So the long and the short of it: unless your doctor has told you otherwise, your hiatal hernia is most likely just something that was found by accident, and not something you need to treat.
The post Highlight on Hiatal Hernia appeared first on Talia Zenlea.
]]>The post Don’t Eat That! appeared first on Talia Zenlea.
]]>
“Food For Thought” is a recurring column on bellyblog.ca, where we will share a well-curated collection of high quality, thought-provoking pieces, usually about food, diet, nutrition, and the gut.
Irritable Bowel Syndrome, or IBS, is a complex syndrome characterized by abdominal pain and altered bowel habits. It’s very common, and can have a major impact on quality of life. Read more about IBS here.
Despite IBS making up about 30% of all consults to a gastroenterologist (in my practice, I’d say it makes up upwards of 75% of all consults!), our understanding of what causes it is still pretty poor. As a result, our treatments often focus on managing the symptoms.
One thing we do know is that for a lot of IBS sufferers, diet plays an important role in causing symptoms, and dietary manipulation is often suggested as a first-line therapy. The most common foods that trigger IBS are dairy, gluten, and FODMAPs, so elimination of these foods commonly recommended. Read more about elimination diets here.
Here’s a fantastic article I wanted to share from a well-respected scientific journal discussion the relationship between food and IBS symptoms. A “must-read” for anyone with IBS, in my opinion.
The post Don’t Eat That! appeared first on Talia Zenlea.
]]>The post Crohn’s Disease appeared first on Talia Zenlea.
]]>
Crohn’s Disease is a form of Inflammatory Bowel Disease, or IBD. The other form of IBD is called Ulcerative Colitis, which you can read about here. Read more about IBD in general here, and remember that IBD is very different from IBS, which stands for Irritable Bowel Syndrome, which you can read about here.
Crohn’s Disease can involve any part of the digestive tract, from mouth to anus. Now that doesn’t mean it DOES involve the whole tract- just that it CAN. The most common part of the digestive tract to be affected by Crohn’s is called the terminal ileum, and it’s the very end of the small bowel, right where it connects to the appendix and large intestine (also called the colon). Some people only have Crohn’s involving the colon, some people have it involving only the small bowel, some people have it involving segments of both. It’s rare, but some people have Crohn’s disease affecting their upper GI tract, like their stomach or esophagus.
Symptoms of Crohn’s can vary, depending on what part of the digestive tract is involved.
Typically, Crohn’s of the ileum or small bowel presents with belly pain and watery diarrhea. If the Crohn’s involves the colon, there can be blood in the stools, or even constipation.
One last point about Crohn’s is that it’s a “full thickness” disease, meaning it involves all layers of the wall of the digestive tract.
If you think of the digestive tract as garden hose running from mouth to anus, it means that the inflammation isn’t limited to the inner lining of the hose – the whole rubber can be affected, and this can sometimes lead to complete breakdown of the wall of the hose. Now the wall of the digestive tract serves a really important function in the body – it keeps poop and bacteria contained. So when there’s loss of integrity of that wall, bacteria can seep out and lead to infections. It can also the make the wall very sticky, and it can stick to other nearby structures within the belly, like the uterus, bladder, or other loops of bowel. These connections are called fistulae and can lead to unique problems of their own. Sometimes these fistulae can pop out to the skin. The skin around the anus, vagina and perineum are particularly susceptible.
When some of these “full thickness” complications heal, they can lead to scarring. Instead of the garden hose, think of the digestive tract as a floppy, deflated balloon. It’s build like this so that it can accommodate “traffic” – digested food and water flowing through it. Once there’s scarring, the wall of the balloon becomes stiff, so when you try to blow it up, that section doesn’t. This is called a stricture, and can lead to food, stool or even air getting stuck, causing what called an obstruction.
Lastly, symptoms of IBD aren’t limited to the digestive tract. IBD can cause fevers, low blood counts and poor nutrition, which can lead to weight loss and feelings of low energy and fatigue. Sometimes people with IBD can develop rashes, skin lesions, and problems with their eyes and joints.
If you are having symptoms or are concerned about IBD, you should consult with you doctor to see if any further testing is warranted.
The Crohn’s and Colitis Foundation of America has a lot of great info on IBD, including treatment options for Crohn’s.
Also check out Amrit’s IBD story on Faces of Healthcare.
The post Crohn’s Disease appeared first on Talia Zenlea.
]]>The post Routine Heath Maintenance for IBD appeared first on Talia Zenlea.
]]>
Routine health maintenance for people with inflammatory bowel disease (IBD) is very important.
IBD consists of Crohn’s Disease and Ulcerative Colitis, which are chronic inflammatory diseases of the digestive tract. Read more about IBD here.
IBD is thought to be an autoimmune disease. Normally, the body produces a whole bunch of cells and proteins, with various different jobs, including fighting infections and protecting the GI tract from harm. The immune systems of people with IBD react inappropriately to these cells and proteins, mistaking them as foreign invaders rather than helpers. Their bodies then mount a strong reaction to this perceived threat, which can result in damage to the digestive tract, which in turn can lead to symptoms.
Because of this, treatments for IBD often focus on suppressing the immune system. Unfortunately, this can mean that the body’s natural defense against infections is weakened. Because of this, your doctor may recommend that you obtain certain vaccines (like a flu shot or a pneumonia vaccine), or have your blood checked for immunity to certain vaccine-preventable disease (like hepatitis A and B).
You may be wondering why your doctor would recommend these if you aren’t on immunosuppressive therapies (or any medications at all) for IBD. The reason is that IBD is a relapsing and remitting disease, meaning most people have periods of no symptoms at all, called remission, alternating with “flare-ups.” Periods of remission can last anywhere from a few months to a few years, and some lucky people with IBD may never have any flare-ups at all. Unfortunately, it’s impossible to know for sure if and when someone with IBD will flare-up. And so your doctor will likely want to make sure that your body is ready and protected if and when the time comes to give you medications that suppress the immune system. The reason your doctor may not want to wait until then is because some vaccines take a while to work (and you may require more than one shot over several months), and vaccines tend to work better when you are healthy and not having a flare-up.
Your doctor may suggest age-appropriate cancer screening, and screening for colon cancer early and more aggressively if you’ve had colitis. They may also suggest skin exams if you are on certain medications that increase your risk of skin cancer.
Finally, people with IBD can be at increased risk for osteoporosis and osteopenia, so you doctor may suggest checking vitamin D levels and doing bone density testing.
For all of these reasons, if you have IBD, it’s really important to see your doctor regularly, even if you feel fine.
Here’s a checklist I use to make sure I don’t forget anything. Feel free to print this out and bring it with you to your doctor’s appointment, or show your doctor the link.
The post Routine Heath Maintenance for IBD appeared first on Talia Zenlea.
]]>The post Ulcerative Colitis appeared first on Talia Zenlea.
]]>
Ulcerative Colitis is a form of Inflammatory Bowel Disease, or IBD. The other form of IBD is called Crohn’s Disease, which you can read about here. Read more about IBD in general here, and remember that IBD is very different from IBS, which stands for Irritable Bowel Syndrome, which you can read about here.
Unlike Crohn’s Disease which can involve any part of the digestive tract, Ulcerative Colitis ONLY involves the large intestine (also called the colon – hence the term “colitis”). Inflammation starts at the rectum, and works its way up. Some people have Ulcerative Colitis that is limited to just a few centimeters within the rectum, while others can have their entire colon involved.
Symptoms can range from urgent and more frequent stools, to full blown bloody diarrhea. Some people experience a spasm feeling in the rectum, like they have to have a bowel movement, but may only pass air, blood or mucous, and even feel constipated.
Lastly, symptoms of IBD aren’t limited to the digestive tract. IBD can cause fevers, low blood counts and poor nutrition, which can lead to weight loss and feelings of low energy and fatigue. Sometimes people with IBD can develop rashes, skin lesions, and problems with their eyes and joints.
If you are having symptoms or are concerned about IBD, you should consult with you doctor to see if any further testing is warranted.
The Crohn’s and Colitis Foundation of America has a lot of great info on IBD, including treatment options for Ulcerative Colitis.
Also check out Amrit’s Ulcerative Colitis story on Faces of Healthcare.
The post Ulcerative Colitis appeared first on Talia Zenlea.
]]>The post Inflammatory Bowel Diseases: The Basics appeared first on Talia Zenlea.
]]>
Inflammatory bowel disease (IBD) consists of Crohn’s Disease and Ulcerative Colitis. IBD is very different from IBS, which stands for Irritable Bowel Syndrome, which you can read about here.
These are chronic inflammatory conditions, meaning they are characterized by episodes of symptoms, alternating with episodes of feeling fine. When people with IBD “feel fine” it means they are in remission – but not “cured” the way you would be of a cold or flu. So it follows that the goal of therapy for people with IBD is to induce remission, and then maintain it for as long as possible.
Crohn’s Disease and Ulcerative Colitis can be associated with a constellation of symptoms, which means that one person’s Crohn’s Disease may not look anything like the next person’s. Check out these posts to learn more about the symptoms and treatments for Crohn’s Disease and Ulcerative Colitis.
We know that IBD is caused by inflammation, likely because of something called an autoimmune process. Normally, the body produces a whole bunch of cells and proteins, with various different jobs, including fighting infections and protecting the GI tract from harm. The immune systems of people with IBD react inappropriately to these cells and proteins, mistaking them as foreign invaders rather than helpers. Their bodies then mount a strong reaction to this perceived threat, which can result in damage to the digestive tract, which in turn can lead to symptoms.
What makes one person develop IBD and not another is still unknown.
We know IBD runs in families, but we also know that that’s not the whole story, and just because your parent or sibling has IBD, it doesn’t mean that you will, and vice versa for them if you have it. So our treatments focus more in controlling the inflammation – we don’t have anything that can stop IBD from developing, or predict who is or isn’t going to have it.
IBD can affect anyone, at any age, of any gender, and from any ethnicity. We know that it’s just as common in men as it is in women. IBD is more common in Caucasians and Ashkenazi Jews, but people of other races and backgrounds can develop IBD, too.
Read more about Crohn’s Disease and Ulcerative Colitis here. The Crohn’s and Colitis Foundation of America has a lot of great info on IBD, including treatment options for Crohn’s and Ulcerative Colitis.
Also check out Amrit’s story on Faces of Healthcare.
The post Inflammatory Bowel Diseases: The Basics appeared first on Talia Zenlea.
]]>The post IBS Is Not IBD appeared first on Talia Zenlea.
]]>
Crohn’s Disease and Ulcerative Colitis are inflammatory diseases of the bowel (IBD, for Inflammatory Bowel Disease).
There’s a lot of confusion out there (among the general public but also among doctors) about what IBD is. Though IBD and IBS (which stands for Irritable Bowel Syndrome) are only one letter apart, they are 2 conditions that could not be more different.
IBS is a condition characterized by symptoms that can be a nuisance for sure, but don’t usually cause major health problems. More info on IBS can be found here.
IBD, on the other hand, is a serious illness that usually requires daily mediation to treat. You can’t diagnose yourself with IBD – it requires some investigations and a good history by a doctor to confirm. If you aren’t sure if your primary care doctor told you had IBD or IBS, chances are, it was IBS… This is something you should absolutely confirm before you meet with any new doctor.
Having IBD is an important part of your medical history, and has implications for your your overall health, cancer screening, what medications other doctors can prescribe to you even for conditions that have nothing to do with the GI tract, and influences how they will interpret some of your laboratory tests.
Another thing worth noting is that sometimes, when doctors are referring to IBD involving the colon, they call it “colitis.” This does not mean that any and all colitis is IBD. Confused yet? Colitis is a general term that describes any inflammation of the colon – that inflammation can be caused a chronic condition (IBD), or it can be caused a whole bunch of other things, like having eaten some bad chicken or drinking the water in Mexico. Often, that colitis resolves on its own or with a short course of treatment – and has nothing to do with IBD.
Crohn’s and Ulcerative Colitis are serious, chronic conditions that require oversight and care from a gastroenterologist. The good news is that there are some good treatment options now, so many people can achieve remission and have long periods of time without any symptoms at all.
To learn more about what it’s like to live with IBD, check out Amrit’s story on Faces of Healthcare.
The post IBS Is Not IBD appeared first on Talia Zenlea.
]]>The post Friend or Foe? Understanding H pylori appeared first on Talia Zenlea.
]]>
Helicobacter pylori (aka H. pylori) is a bug that lives in the stomach, and thrives in the acidic environment.
It’s the most common chronic bacterial infection in humans, and amazingly, about a third of north American and north European adults are infected.
In areas such as South America and Asia, rates of infection are higher than 50%!
Why is this important?
H. pylori can cause ulcers, as well as inflammation of the stomach (called gastritis), which in turn can cause discomfort (called dyspepsia). Over time (we’re talking years here usually), it has clearly been associated with various forms of stomach cancer. But don’t worry – most people with H. pylori DO NOT get stomach cancer, and in fact live their lives without ever knowing they had it in the first place.
How do I get tested?
The best tests to look for active infection are a breath test or a stool test. A blood antibody test is also available; however, once you’ve tested positive, you will always be positive, even if you’ve been treated and cleared the infection. We can also detect active infection with stomach biopsies taken during an endoscopy.
How did I get this?
Sorry to gross you out – but H. pylori is contracted by ingesting poop from an infected person. And it’s not as impossible at it sounds – any unsanitary practices, like poor hand hygiene, can lead to tiny amount of infected stool being passed from hands to mouthes of strangers. It can also be transmitted orally through saliva.
How do I get rid of it?
The good news is, treatment is very easy. It involves a combination of antibiotics and acid reducing medications (proton pump inhibitors). Your doctor will advise you on which ones to take based on your history.
Can I get reinfected?
Yes, but it’s very, very unlikely.
The post Friend or Foe? Understanding H pylori appeared first on Talia Zenlea.
]]>The post Accidents Happen: A Fecal Incontinence Primer appeared first on Talia Zenlea.
]]>
Having “an accident” as an adult can be extremely embarrassing – something you might not even feel comfortable discussing with your doctor. Know that you aren’t alone. It’s estimated that about 5% of women over the age of 60 will have experienced an involuntary loss of stool.
This can arise from any number of medical conditions that weaken the body’s ability to hold stool in, such as diabetes mellitus, multiple sclerosis, dementia, and spinal cord injuries, just to name a few.
But did you know that even pregnancies and childbirth that may have happened many years prior can lead to incontinence of stool decades down the road?
You might be especially at risk if you had a vaginal delivery, particularly one with known trauma to the anal sphincter, or one that required forceps. Big babies (especially those over 9.5 pounds) can also put you at increased risk for troubles down the road.
Another surprising reason some women have fecal incontinence is chronic constipation. Though it seems counterintuitive, hard stool sitting in the rectum for prolonged periods of time can actually result in overflow of loose stool, and even relaxation of the sphincter, or muscle that holds stool in, resulting in incontinence of even formed or hard stool.
Depending on the cause of the incontinence, there are various treatment or management options that exist. So don’t suffer in silence, and don’t be embarrassed to bring this up with your doctor. The sooner you do, the better, especially if you are older than 40, or have chronic diarrhea or risk factors for colorectal cancer. Take control of your symptoms before they take control of you.
The post Accidents Happen: A Fecal Incontinence Primer appeared first on Talia Zenlea.
]]>